Why Calling 9-1-1 Could Save Your Life During a Heart Emergency
January 20, 2026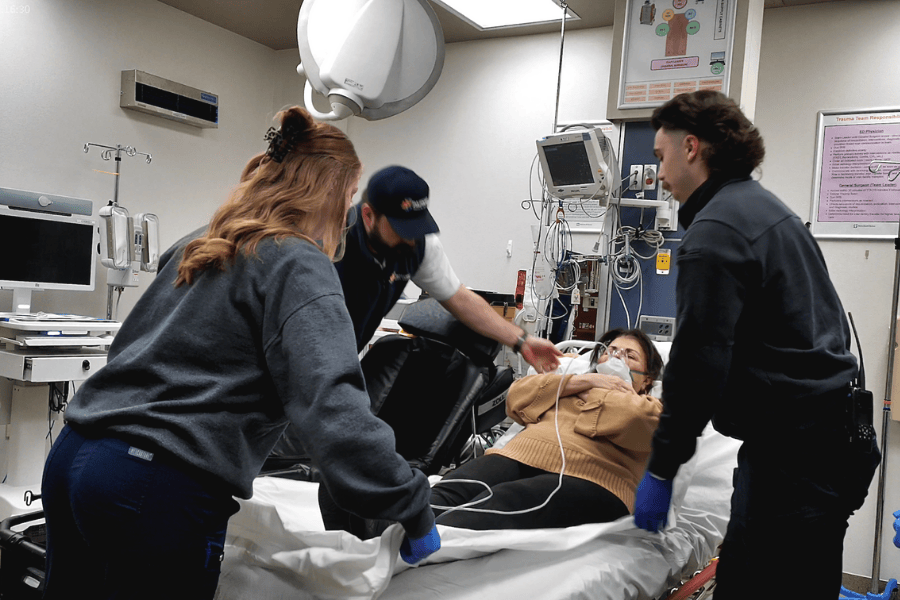
By Ayman Alshami, MD
It’s late in the day, and something doesn’t feel right. There’s a tight pressure in your chest that won’t quite go away. Maybe it’s stress, maybe indigestion — but as the minutes pass, you begin to wonder what you should do next. Should you wait it out? Should you drive yourself to the hospital? Or should you call 9-1-1?
That moment of decision can be one of the most important during a heart emergency. Many people choose to drive themselves or get a ride from friends and/or family, believing it will be faster. While that choice may seem practical, it can also be dangerous.
As an interventional cardiologist, I want people to understand that calling 9-1-1 during a possible heart attack is the safest and most effective option — even if you live far from town or think you can make it to the hospital on your own. I recently joined Saline Health System and care for patients at Saline Cardiology. In my role, I treat patients who need urgent, time-sensitive heart procedures, and I see firsthand how the first decisions made during a heart emergency can directly affect outcomes.
Minutes matter in a heart attack
During a heart attack, blood flow to part of the heart muscle is blocked. The longer that blockage remains, the more damage occurs. This is why we often say “time is muscle.” Every minute without treatment increases the risk of permanent heart damage or death.
EMS care starts before you reach the hospital
Calling 9-1-1 allows emergency medical services to begin care immediately, long before you reach the hospital. Paramedics can administer oxygen, give medications such as aspirin to help reduce clot formation and, when appropriate, nitroglycerin to improve blood flow and relieve chest pain.
They will also check vital signs and can perform an electrocardiogram, or EKG, in the field. The paramedics then continuously monitor heart rhythm and vital signs, allowing them to respond quickly if complications arise.
At the same time, EMS teams communicate with the hospital so the care team is ready before you arrive. This early notice allows medications and equipment to be prepared and the appropriate specialists to be in place. Rather than spending critical time organizing care after you arrive, treatment can begin right away.
Know when to call
Not all heart attacks feel the same. Some are sudden and intense, while others begin with milder symptoms that worsen over time. Call 9-1-1 right away if you or someone with you experiences chest discomfort that lasts more than a few minutes or comes and goes. This may feel like pressure, squeezing, fullness or pain.
Other warning signs include discomfort in one or both arms, the back, neck, jaw or stomach, shortness of breath with or without chest pain, cold sweats, nausea or lightheadedness. If something does not feel right, trust your instincts and call for help.
When in doubt, make the call
I often tell patients that it is better to call 9-1-1 and learn it was not a heart attack than to delay care during a real emergency. No one will be upset that you called. Emergency responders are there to help, and they would rather evaluate a concern early than arrive too late.
Heart emergencies are unpredictable, but how you respond does not have to be. Calling 9-1-1 is one of the most important decisions you can make to protect your heart and your life.
At Saline Health System, our team is committed to providing timely, compassionate care when it matters most. If you would like to talk with a provider about your heart health or risk factors, we can help. Visit the “Find a Doctor” tab at SalineMemorial.org or call 501.387.0163 to connect with a provider. In the event of a heart-related emergency, call 9-1-1 immediately. Acting quickly may save a life.
